- Embryotools has achieved the birth of the world’s first foal conceived using the pioneering technique maternal spindle transfer. Unlike egg donation, this technology allows the mother to contribute to the genetics of the offspring produced, offering new perspectives for lineage preservation and species conservation.
- This experimental technique has already demonstrated its efficacy as a treatment for infertility in humans with the birth of seven healthy babies for couples who had been unable to conceive despite numerous IVF treatments. The clinical results emphasize the potential of maternal spindle transfer as a solution to poor egg quality, both in veterinary and human medicine.
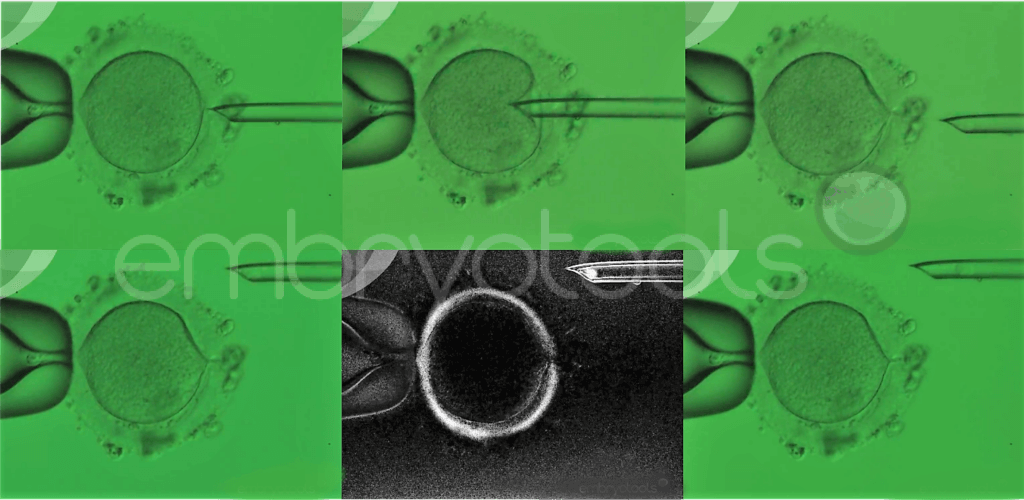
- Maternal spindle transfer, commonly known as the “three-parent technique,” involves placing the mother’s DNA into a high-quality egg from a fertile donor, which is then fertilized with the father’s sperm, improving the egg’s quality and increasing the chances of a successful pregnancy.
- Following the success of this birth, accomplished together with researchers from Oxford University and Ghent University, Embryotools aims to promote changes in the current legislation to consolidate a legal, ethical and scientific pathway for the use of maternal spindle transfer to prevent mitochondrial genetic diseases and treat incurable cases of infertility associated with poor oocyte quality.
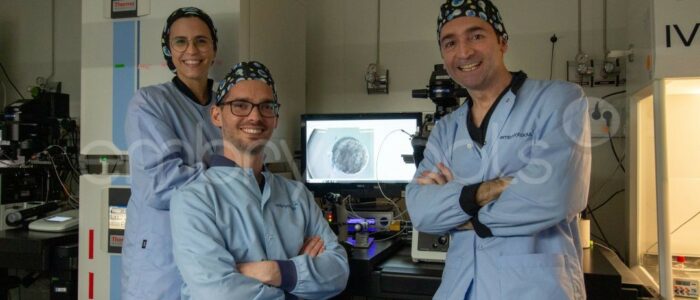
Barcelona, 9 September 2025. Embryotools, a biotechnology centre based at the Parc Científic de Barcelona (PCB), has achieved a new milestone in the field of assisted reproduction with the birth of the world’s first foal following maternal spindle transfer (MST). For ten years, the laboratory has been leading the development of mitochondrial replacement therapies, applying novel and innovative technologies to solve complex problems of infertility and inherited disease. The efficacy of MST in humans has recently been demonstrated with the birth of seven babies to women with severe infertility and a long history of unsuccessful IVF treatments. Now, for the first time, MST has been successfully applied to horses.
This breakthrough marks a milestone in equine reproduction, as it makes it possible to preserve and transmit the DNA of competition horses, whose genetic material could not otherwise be propagated due to infertility. Unlike egg donation, the technique keeps the maternal genetic contribution intact, opening up new opportunities for lineage preservation and species conservation.
“The success of the technique in both humans and horses confirms that this is a solid, reproducible reproductive tool with enormous clinical potential. In humans, it has allowed the birth of healthy children in situations where the only alternative was egg donation. In horses, it has proven useful in mares with a long history of failed cycles, which reinforces its value even in contexts where genetics is especially relevant, such as high-value animal reproduction,” said Dr Nuno Costa-Borges, co-founder and scientific director of Embryotools.
MST, originally used to prevent the transmission of mitochondrial diseases, has proven effective in the treatment of infertility associated with poor egg quality. While MST has sometimes been referred to as a “three-parent technique”, Embryotools rejects the term as misleading and lacking in scientific rigour. Dr Costa-Borges explains that “while it is true that the technique involves the use of mitochondria from a third individual, what is transferred is only a tiny amount of mitochondrial DNA, which represents less than 0.1% of the total genome – and does not contribute to the physical characteristics or personal traits of the future embryo. The entirety of the nuclear genetic material, which determines the biological identity of the individual, comes exclusively from the two parents”. “To suggest that there are three parents would be like saying that a person who has received a heart, liver or bone marrow transplant has an additional parent, which obviously is not a consideration, medically or ethically”.
Researchers at Oxford University confirmed through genetic analysis the feasibility of the procedure in horses and its potential to improve reproduction, especially in animals with high genetic value or reduced fertility. Dr Dagan Wells, a leader in reproductive genetics from Oxford, highlighted the relevance of this advance. “This has been a remarkable and highly successful team effort, combining cutting-edge methods in embryology, genetics and veterinary medicine. The work adds to a growing body of evidence indicating that the MST method, which the Embryotools team has gone a long way towards perfecting, can serve as an effective treatment for otherwise incurable forms of infertility. The technology is likely to have an important role in the conservation of critically endangered species, helping to preserve the genetic diversity essential for viable populations by allowing more females to pass on their genes to future generations”.
In collaboration with Dr Katrien Smits and Dr Jan Govaere, from Ghent University, and Dr Margot Van de Velde from the Belgian Dymart Equine Fertility Center, the birth of this foal in Belgium represents a milestone in the clinical validation of MST as an effective method to treat complex infertility cases, opening up new opportunities in assisted reproduction.
The results of this study were presented last week by Mònica Acacio, head of Embryotools’ equine reproduction unit, at the 41st Annual Scientific Meeting of the Association of Embryo Technology in Europe (AETE), held in Cork (Ireland).
A key tool for lineage and biodiversity preservation
In equine breeding, genetics is everything. Horses descended from champions not only stand out for their performance but have a high market value. For this reason, assisted reproduction in competition horses has become a strategic tool, especially in disciplines such as show jumping, polo, dressage and racing. Its objective is clear: preserve elite genetics and reduce the risks inherent in traditional breeding.
In this context, MST offers an innovative solution for mares with severe infertility, as it allows their genetics to be passed on to future generations even when other methods have failed. The same method also has the capacity to avoid the transmission of mitochondrial diseases, a group of hereditary disorders that are transmitted exclusively maternally through mitochondrial DNA.
The first mare to benefit from this pioneering technique was Flow, a Belgian dressage champion of exceptional genetic value, owned by Anthony Detroyer, who, together with his colleague Davy Van De Moere, breeds dressage horses and runs a private sport stable. “For Flow, we had previously tried numerous techniques without success. While searching for alternatives, we came across a study by Embryotools, which had successfully addressed similar issues in humans. We reached out to them, and a few months later, we set the process in motion. We are overjoyed with the birth of this new foal, a true milestone for both our stable and the future of dressage breeding”, affirms Van De Moere.
The Embryotools team was able to create viable embryos from Flow’s genetic material and donor oocytes from another fertile mare. One of the embryos was transferred to the recipient who, after a complete gestation, gave birth in June 2025 to the world’s first foal conceived thanks to this technique.
This milestone opens up new avenues in equine reproduction for the preservation of valuable lineages in animal husbandry. It may also prove particularly beneficial in the conservation of other animal species.
“Our goal is to continue exploring the potential of this technique and to continue developing studies that will allow us to accumulate solid evidence on its efficacy and safety, since it is a technique that is still considered experimental, although with enormous potential. The success in the animal model of the horse, where genetics plays a key role, again proves the reproductive value of the technique in a context different from the human one, but equally demanding”, said Dr Costa-Borges.
Proven clinical success with the birth of seven babies
In 2023, Embryotools led the world’s first clinical study on MST as a treatment for idiopathic infertility, conducted in Greece. The research concluded with the birth of seven babies from patients with a long history of unsuccessful IVF attempts, affirming this technique’s potential in reproductive medicine.
In light of these results, Embryotools’ objective is to “continue to gather scientific evidence that will allow us to evaluate its efficacy and safety with greater precision, and to move towards its clinical validation with the support of regulatory authorities,” said Dr Costa-Borges. “We are currently actively promoting this work and seeking the support of scientific and regulatory authorities so that Spain is not left behind in this field”.
In the same vein, a recent study by scientists at Newcastle University in the UK achieved the birth of eight babies through pronuclear transfer, another mitochondrial replacement technique that, unlike maternal spindle transfer, exchanges nuclear DNA between already fertilized embryos to combine the donor’s healthy mitochondria with the biological parents’ genetic material. Both approaches have shown promising clinical results and good safety, reinforcing their potential in advancing reproductive medicine.
A consolidated centre with more than 30 years of experience in embryology
Embryotools has a consolidated scientific track record with more than 30 years of experience and state-of-the-art laboratories, which allows it to offer advanced reproductive solutions to breeders worldwide, both to solve infertility cases and to optimise reproduction in high-performance horses. The combination of cutting-edge science with practical clinical and veterinary applications has made the centre an international benchmark in both human and animal reproduction.